80 year old female with gastric complaints
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solveb those patient's clinical problems with collective current best evidence based inputs.
This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box is welcome.
CASE:
This is a case of a 80 year old female with complaints of
1. vomitings (4-5 episodes)
2. abdominal discomfort since 08/04/2023.
HISTORY OF PRESENTING ILLNESS:
Patient was apparently asymptomatic 2 hours ago.She then had 4-5 episodes of vomiting which contained of food particles,non bile stained,not foul smelling and not blood stained.It is associated with giddiness and abdominal discomfort.
No complaints of fever,loose stools,shortness of breath,chest pain,orthopnea.
H/O consumption of alcohol 1 day back.
PAST HISTORY:
H/O similar complaints of giddiness and neck pain present.
K/c/o cervical spondylosis
H/O travel to USA (stayed there for 5 months) and she returned back 1 week ago.
H/O upper GI endoscopy done 10 years ago for gastric ulcers and is on medication.
Not a k/c/o HTN,DM,CVA,CAD,TB,Asthma
PERSONAL HISTORY:
Diet:vegetarian
Apetite: normal
Sleep:decreased
Bowel and bladder:regular
Addictions: drinks toddy occasionally; she had one glass yesterday (08/04/2023).
GENERAL EXAMINATION:
Patient is drowsy,coherant and cooperative
No pallor,icterus,cyanosis,clubbing,lymphadenopathy and pedal edema.
Vitals:
BP:130/80 mmHg
Temperature: afebrile
PR:80bpm
RR:30cpm
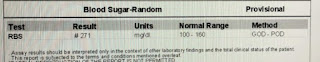
GRBS:281 mg/dl
SYSTEMIC EXAMINATION:
CVS: S1 and S2 are heard
CNS: no focal neurological deficits
Abdomen: soft,obese and non tender
RS: B/L inspiratory fine basal crepts
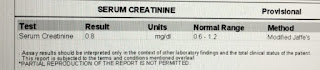
INVESTIGATIONS:
TREATMENT:
- Inj.Augmentin 1.2g/IV/BD
- Tab. Metformin 500mg/PO/BD
- Tab.Lasix 20mg PO/BD
- Inj Pan 40mg/PO/BD
- SYP.Grilinctus 2Tbsp PO/TID
- nebulization
Ipravent -6th hourly, budecort -8th hourly
Mucomist-12th hourly
- GRBS monitoring 6th hourly
- Chest physiotherapy
PROVISIONAL DIAGNOSIS:
B/L lower lobe consolidation (with community acquired pneumonia)
With Heart failure
With preserved ejection fraction (58%)
With denovo DM Type 2




























Comments
Post a Comment