38 year old male with chronic liver disease
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solveb those patient's clinical problems with collective current best evidence based inputs.
Patient was apparently asymptomatic 9 months back then he developed jaundice with yellowish discoloration of eyes and urine , associated with pruritis for which he went for evaluation and upper GI endoscopy was done on 12/7/22 and given impression of low grade esophageal varices,mild PHG since then he is having similar episodes of jaundice once in a while and usg was done multiple times
Usg impression on 6/12/22 :- moderate hepatosplenomegaly ,gall bladder sludge ,no evidence of choledocholithiasis ,b/l minimal pleural effusion (rt>lt),minimal ascities visualized .
On 14/12/22 usg impression:- moderate hepatosplenomegaly with fatty liver , altered echo texture to rule out cld changes ,mild intra heptaic biliary reticular dilatation in left lobe of liver ,gn sludge ,mild splenomegaly ,mild IHBRD noted in the left lobe of liver.
On 18/2/23 :-
On 18/02/2023 He presented to another hospital with complaints of Productive cough, streaky (blood) sputum, intermittent fever spikes with chills & rigors. Patient was admitted there for further management.
Patient was started on IV antibiotics, PPI, antifibrinolytics, nebulisation and other supportive care. All necessary investigations were done. Na*: 129. PT / IN - 20.5/1.49, Fibrinogen - 499, Total bilirubin - 8.4. CT chest aortogram was done which showed B/L tree in bud with diffuse GGO. Sputum was sent for analysis. Dengue IgM was positive. Repeat CBP showed PCV - 24, Hb - 9.10, TLC - 6150. General physician consultation was taken in view of Dengue and continued on medical management. Hepatologist consultation was taken and advised for medical management. Patient was discharged in stable condition with the following advice.
-Tab. Doxycycline 100mg twice daily for 5 days -Tab. Pan 40mg once daily at 7am (½hr before breakfast) for 5 days
-Tab. Mondeslor 1 tab once daily at 7pm for 5 days
-Syp. Ascoril - D 10ml thrice daily
-Tab. Udiliv 300mg 2tab twice daily
Patient was on alcoholic abstinence since then and symptoms gradually decreased but since 3 days patient was on alcohol binge and vomitings started from 3rd day night that is from 6/4/23 to 7/4/23, 10-15 episodes of vomitings which were non bilious,non projectile , didn't contain food particals, mucous gelly like consistency, one of the episode contained brownish black jelly like material at the end of the episode associated with mild abdominal pain .
Past history:- Not a known case of DM,HTN,TB, Asthma, epilepsy
Personal history:-
Diet-mixed
Appetite:- reduced since 3 days
Sleep :- adequate
Bowel and bladder movement-regular
Addictions:- drinks alcohol since 20 years
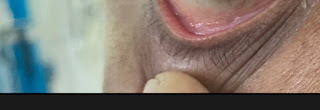
General examination:-
Patient is conscious, coherent,cooperative
Well built and well nourished
No Pallor, icterus, clubbing, cyanosis, generalized lymphadenopathy, bilateral pedal edema.
Vitals:-
BP:- 140/80 mmhg
PR:- 86BPM
Temp :- afebrile
Grbs:- 105 mg/dl
RR:- 16 cpm
Systemic examination:-
Cvs:- s1 s2 present,no added sounds/murmurs, jvp not raised
RS :- bilateral air entry
Investigations:-
Provisional diagnosis:- chronic decompensated liver disease with h/o hepatosplenomegaly with low grade esophageal varices with h/o hypertension
Treatment:-
1.IVF one print NS, one print RL @50ml/hr
2.salt restriction <2gm/day
3.protein rich diet ( 2 egg whites /day ,2 scoops of protein powder in 100 ml glass milk)
4.INJ.PAN 40 mg/iv/od
5.INJ.thiamine 200mg/iv/bd
6.INJ.Zofer 4g/iv/tid
7.INJ Neomol 1g/iv/if temp >101F (sos)
8.tab.dolo 650mg/po/bd (sos)
9.syp. lactulose 15ml/po/bd
11.syp. potklor 10 ml in 1 glass of water /po/bd
12.monitor vitals BP,Temp,RR,PR, Saturation
13.tepid sponging
14.tab. CINOD 10mg/po/od
15.strict I/O charting























Comments
Post a Comment