35 year old male with uncontrolled sugars
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment
Case:
35 year old male farmer by occupation is brought to opd with
C/O vomiting since 8 days.
History of presenting illness:-
Patient was apparently asymptomatic one month back. He then has occasional episodes of vomitings which are increased in frequency since past 8 days that is of 1 - 2 episodes per day,Non projectile,Non bilious,Not blood tinged,Food particles as content associated with fever,Not associated with pain abdomen
8 months back patient suffered with ? Chickenpox for 1.5 month .
2months after recovery from chicken pox he is diagnosed as having DM (probably type 1)when patient presented with unconscious state
H/o of shortness of breath( grade 2) for 1 month which is intermittent ( increased during night),Associated with cough and fever
Burning micturation present
Cough initially Non productive later productive ,Associated with scanty sputum,Non blood tinged
Fever is low grade, intermittent,associated with night sweats not associated with chills and rigors
Weight loss (8 to 10 kg) from past 3 months
Progressive increase in weakness which is increased in severity since past 10days
Decreased appetite since past 1 month
Since 4months he was on Mixtard 10 units once daily for his DM
But Patient stopped takimg medication since 1 month
N/k/c/o htn asthma,CAD,TB,epilepsy
Non alcoholic,Non smoker,No relevant family history
Treated outside for UTI - ecoli with antibiotics
Vitals -
Bp:- 140/80 mmHg
PR :-123bpm.
Sat- 100 on RA
Grbs - High at presentation
RR- 26cpm
Temp- 100°F
Systemic examination:-
Cvs - S1S2
Rs- B/L air entry present
Started on ivf NS bolus f/b 75ml/hr
Inj Hai 6u IV hourly---> infusion @6u/hr
2d echo - ivc 1.28cm ,collapsible
Normal chambers
Mild lvh
Hemogram:-
Hb-7.2
TLc- 22,800
Plt- 3.3 lakhs
Microcytic hypochromic
Urea-206
Creat 4.0
Na-131
K-4.7
Cl- 95
Urine for ketones negative
Rbs- 485 mg/dl
Course in the hospital:- patient presented to our hospital with the above mentioned complaints, thorough clinical and metabolic evaluation was done.
GRBS was high, RBS was 485mg/dl, urine for ketones was negative and ABG showed metabolic acidosis
Patient was treated for uncontrolled sugars with insulin Inj.Hai @6ml/hr infusion and tapered the insulin according to the GRBS blood sugar levels were controlled.
As the patient was having recurrent Urinary tract infections and fever spikes USG abdomen was done which showed b/l bulky kidneys with altered echo texture suggestive of pyelonephritis and left sided hydroureteronephrosis .
Urology opinion was taken ivo bilateral pyelonephritis and CT-KUB was advised , IV Antibiotics Inj.Piptaz 2.25gm /IV/TID was given for 4days
Ophthalmology referral done showed :- mild NPDR changes noted and adviced strict glycemic control, review to opthalmology opinion for every 6 months,
Date-12/4/23 Urine culture report showed methicillin sensitivity staphylococcus aureus resistance to penicillins and sensitivity to co trimaxazole ,….and I/v/o renal failure creatinine clearnce 23ml/hr cotrimoxazole (Dose adjustement was done(50%of regular dose) was given for 5 days .
I/v/o anaemia evaluation was done, Hb-7.2 gm/dl,Microcytic hypo chronic ,Reticount :-0.5
Stool for occult blood( + )
Surgery opinion was taken I/v/o previous h/o hemorrhoids and constipation
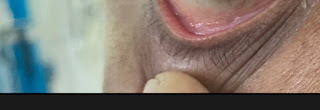
P/R examination showed - skin around the glutial clefts normal
-no external skin tags, fissures, haemorrhoids, sinuses or fistulas
-surrounding external skin stained with stool .
-anal tone is normal
-hard stoll pellets found in the rectum
- all stool pellets have been cleaned upto the level of finger insertion.
-glove stained with dark yellow coloured stool
Adviced - syp cremaffin 30ml/po/hs
-proctoscopy after soap water enema
- advice colonoscopy to rule out losses ,gi bleed
-upper GI endoscopy i/v/o any upper GI bleed
Upper GI endoscopy was planned I/v/o any upper GI bleed which showed esophageal candidiasis, bile reflux gastritis
Endocrinology opinion was taken and was suggested Inj Lantus 10 units at @10pm
Urology opinion was taken again and Fosfomycin 3gm sachets alternative days for 1 week (3 doses) if patient did not improve symptomatically.
Nephrology opinion was taken for presence of ? Diabetic nephropathy and was suggested tab lasix 20mg PO OD for 3days
INVESTIGATIONS :-
Hemogram:-
Hb:- 7.2----6.2----6.8----6.0--6.0
Pcv:- 22.5----20.4----22.5----19.9--19.9
TLC:- 22,800----14,480---9,500----7500-- 7300
RBC:- 3.3----2.89----3.16----2.81--2.78
Platelets:-4.2----3.47----4.0----4.18--4.10
RETICULOCYTE COUNT :- 0.5
RFT :-
Blood urea:- 206----147----77----60--35
Sr creatinine:- 4.0----3.4----2.3----2.3--2.6
S.Na:- 131----139----137----139--139
S.K:- 4.7----4.0----3.8----3.8--3.7
S.Cl:- 95----104----106----104
Ionized Ca:- 1.04--1.08--1.07--1.13
LFT:-
Total bilirubin:- 1.04
Direct bilirubin:- 0.23
SGPT:- 14
SGOT:-11
ALP:- 284
TOTAL PROTEIN:- 8.0
Albumin :- 2.5
A/G ration:- 0.45
24 hour URINARY ELECTROLYTES:-
Na:- 176
Ca :- 297
Phosphorous:-0.87
USG report:-
Review USG:-
2D echo report:-
Upper GI endoscopy:-
Chest x ray:-
ECG:-
CT:-
Report
C& S blood and urine:-
DIAGNOSIS:-
Uncontrolled sugars secondary to non compliance to medication. (Resolved )
Acute kidney injury secondary to? Pre renal secondary to ? Sepsis ?
bilateral pyelonephritis with left hydroureteronephrosis
with anemia (microcytic hypochromic) secondary to?
GI losses
? Iron deficiency anemia
Treatment Given :-
1.IVF- NS @ 75ml/hr
2.Insulin infusion @8 U/hr increase or decrease acc to GRBS(algorithm 2)
3.GRBS charting hourly and inform PG
4.Monitor Temp, PR,RR,BP hourly
5.Strict input output charting.
6.trimethoprim + sulphamethoxazole is given for 5 days starting from 16th


















Comments
Post a Comment