A 49 year old female with joint pains
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box is welcome.
CASE:
A 49 year old female came with chief complaints of pain in the joints since 10 years.
HISTORY OF PRESENTING ILLNESS:
Patient was apparently asymptomatic 10 years back.She then developed fever (on and off type) for which she takes paracetamol (2-3 everyday).She had 2-3 episodes of vomiting,headache and increased frequency of micturation(15-20 times a day).
She then developed pain and swelling in her wrist,ankle,shoulder,elbow,hip,metacarpal phalanges,metatarsal joints and lower back which is radiating to both her legs till feet for which she was taken to the hospital.The medication prescribed to her provided her temporary relief.
She also complaints of pedal edema and stiffness in the joints as soon as she wakes up in the morning.
She has stopped her medication one month back.
DAILY ROUTINE:
She wakes up at 6:00 am in the morning.She takes a head shower everyday as she believes that it reduces her headache.She does the household chores,gets groceries and cooks food.She works at her farm from afternoon to evening and occasionally sells the produce in the market.Later in the night she cooks dinner and sleeps by 8:00pm.
PAST HISTORY:
Not a known case of Diabetes mellitus,Hypertension,Asthma,epilepsy
PERSONAL HISTORY:
Diet: used to have a mixed diet but now she stopped consuming meat
Apetite: decreased apetite
Sleep: reduced
Increased frequency of micturation(15-20 times a day)
Addictions: none
GENERAL PHYSICAL EXAMINATION:
Pallor:present
Icterus:absent
Cyanosis:absent
Clubbing:absent
Lymphadenopathy:absent
Edema: no pedal edema present at the time of examination
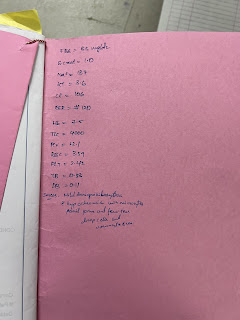
VITALS:
Temperature:100.9 degree fahrenheit at the time of examination
Pulse:70 bpm
Respiratory rate: 24cpm
BP: 110/70 mm hg
SYSTEMIC EXAMINATION:
CVS: S1 and S2 are heard and no murmurs are heard.
RS: Bilateral vesicular breath sounds are normal
CNS: no focal neurological deficits
Abdomen: soft and non tender
EXAMINATION OF THE JOINTS:
Wrist joint: partial movement of flexion and extension
Shoulder joint: she can lift her shoulders but not straight above her head at shoulder joint
Elbow: she can flex and extend normally
Knee and ankle joint: unable to flex completely
INVESTIGATIONS:
On 07/07/2022, Patient had complained of pain and tenderness in both the breast.
DIAGNOSIS:
Rheumatoid arthritis with Chronic anemia
TREATMENT:
Tab prednisolone 100mg OD
Tab Methotrexate 7.5mg weekly
Tab folic acid 5mg
Tab naproxen 250mg TID
Tab amitryptalin 10mg
DISCHARGE SUMMARY:






















Comments
Post a Comment