A 37 year old male with fullness of abdomen since 2 years
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box is welcome.
CASE:
A 37 year old male came with chief complaints of fullness of abdomen since 2 years.
HISTORY OF PRESENTING ILLNESS:
Patient was apparently asymptomatic 2 years back.
He then developed belching and burning sensation in the throat and retrosternal region after consuming spicy and fast foods for which he takes antacids everyday to provide relief.Sometimes he complaints of heaviness in the chest.
Sometimes when he consumes spicy food, he takes antacids and when they do not provide relief,he induces vomiting as there is pain and burning sensation in the chest.
DAILY ROUTINE:
He wakes up in the morning around 9 am.He takes an antacid and has his breakfast.He goes to work (he owns a grocery store) at 10am and returns home and has his lunch between 2-4pm and rests for an hour.In the evening he has snacks and goes back to work.At night he returns home at 10pm and has dinner.He goes to bed around 12am.
Patient consumes green tea/black coffee twice a day.
Occasionally,in the morning before breakfast he takes an antacid and takes his other medication (anti hypertensives),he feels bloated and for relief he takes another antacid.
PAST HISTORY:
Not a known case of diabetes mellitus,asthma,epilepsy.
Patient is a known case of Hypertension since 2012.
One day he felt lightheaded and fatigue.He went to a local clinician and he was diagnosed with HTN.Since then he has been on anti-hypertensives.
In 2015, He said that he was having trouble passing stool.2 days later,he felt an uncomfortable pressure and squeezing type of pain in the chest which lasted for an hour and had subsided on his own.On the day of his heart attack he had sweets and chicken for lunch. After some time he started having pain in the retrosternal region and he induced vomiting and took an antacid to provide relief.In the evening he went to the hospital as he was having hiccups which were not not subsiding and the clinician had advised him for an ECG.
He went to Silguri and got an angiogram done.A coronary artery block was detected and the doctor had given him medication.
In 2016, he had met with an accident for which he had a fracture in the humerus and was on rest for 2 months.
In 2017, he had visited another hospital in Puttaparthi for his treatment (HTN)and regular check up.
In 2021 September, the doctor had decided to do percutaneous transluminal coronary angioplasty (PTCA) to the patient.
PERSONAL HISTORY:
Sleep:normal
Diet: mixed diet
Apetite: Patient feels hungry but he is scared to eat due to bloating.
Bowel and bladder movements: regular
Addictions: Patient has a history of smoking 10-15 years back (6-7 cigarettes a day). He used to drink alcohol 250 ml 2-3 times/week. Patient has completely stopped smoking and drinking since 9 months.
Increase in weight since 2 years.
FAMILY HISTORY:
Patient’s father had a history of hypertension and died at the age of 65. He had undergone bypass surgery. His father also has a history of bloating and belching.
He was paralyzed and bedridden for 8-9 years until his death.
Patient’s mother has a history of HTN and diabetes.
GENERAL EXAMINATION:
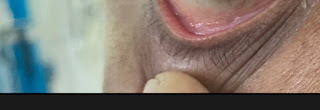
Pallor: present
Icterus:absent
Cyanosis:absent
Clubbing:absent
Lymphadenopathy:absent
Pedal edema: absent
VITALS:
Temperature:98.4 degree farenheit
Pulse:76 bpm
BP:110/80 mm hg
Respiratory rate: 15 cpm
SYSTEMIC EXAMINATION:
CVS: S1 and S2 are heard
CNS: no focal neurological deficits
Abdomen: distended abdomen,soft and non tender
RS: bilateral vesicular breath sounds are heard
INVESTIGATIONS:
PTCA REPORTS:
PROVISIONAL DIAGNOSIS:
Non ulcer dyspepsia with history of PTCA
TREATMENT:
Tab. Clopilet A Twice daily for 3 months and after 3 months once daily.
Tab.Supermet 25mg
Tab.Atocor 40mg OD
Tab.Telmikind 40mg OD
Tab. Sorbitrate 5mg
Source of past history: https://ssahamedicalcases.blogspot.com/2022/07/37-year-old-male-heart-patient-with.html?m=1















Comments
Post a Comment